Blog
Workplace violence in healthcare
Note: This is part of a three-part series on workplace violence in hospitals. Don’t miss the post on resources to help develop programs or support legislation needed to decrease healthcare workplace violence. This post dives into how communication technology can help protect your healthcare staff.
A 2019 AMN Healthcare survey of 20,000 registered nurses found 41% of RNs are victims of bullying, incivility, or other forms of workplace violence. Another 27% say they’ve witnessed workplace violence. The survey adds that more value on safety practices is an opportunity for progress.
Not only are hospital workplace injuries caused by lifting, carrying, and transferring patients, but nurses and other healthcare staff face unique risks not found in other professions, including exposure to chemicals, needle sticks, and the potential for violence from patients and their families.
Violence against nurses and other hospital staff
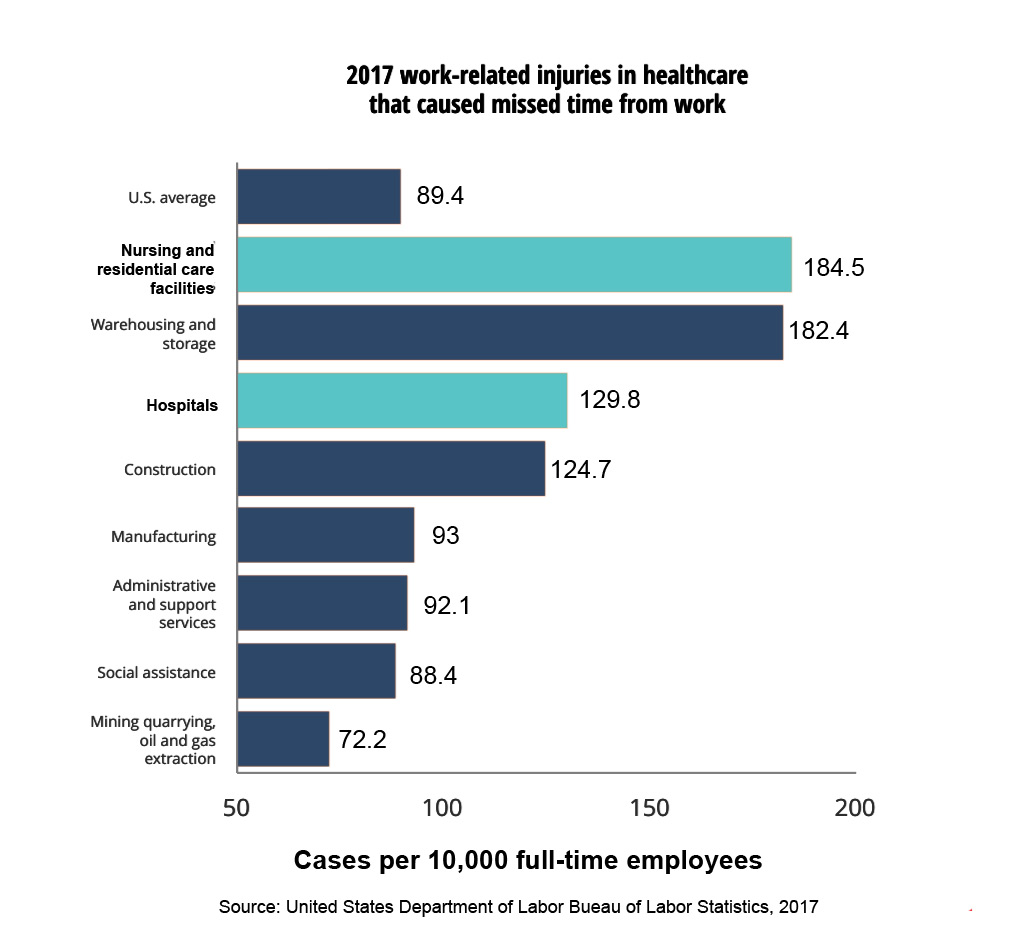
In 2017, hospital staff suffered 51,380 work-related injuries and illnesses that caused employees to miss work. These injuries occurred at an incidence rate of 129.8 cases per 10,000 full-time workers—45% higher than the rate for all occupations (89.4 cases per 10,000 workers).
In terms of employees missing work due to injury or illness, it’s more hazardous to work in a hospital than in construction or manufacturing. Additionally, these numbers don’t account for injuries that go unreported or when an employee continues to work despite an injury.
The causes of injury: What role does violence against nurses and other hospital staff play?
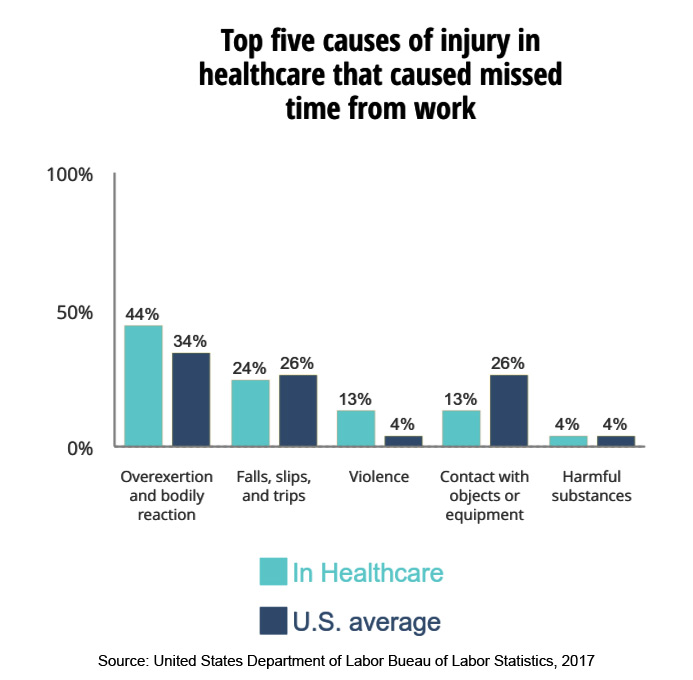
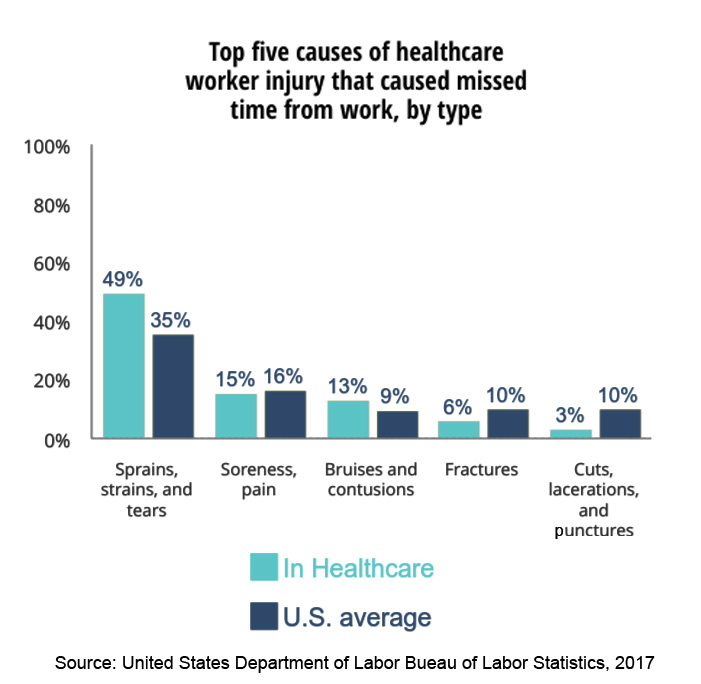
The most common injuries are caused by overexertion and bodily reactions, including motions of lifting, lowering, or repetitive motions. Sprains, strains, and tears are the most common symptoms that require time off from work. These injuries are likely related to patient handling.
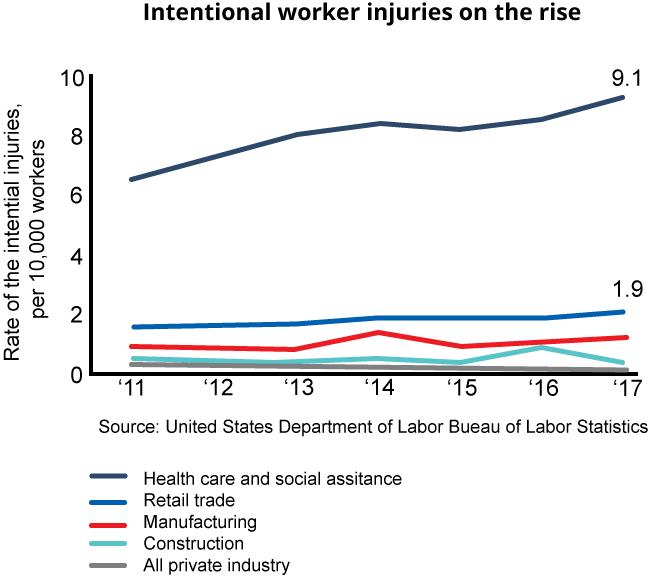
Since 2011, reports of violence increased from 9% to 13%, and are 9% higher than the rate of all U.S. occupations (4%). Again, these numbers don’t account for violent injuries that go unreported or where an employee continues to work despite an injury.
Other research has shown the rate of violence for those in healthcare is as much as twelve times higher than for those in other professions. A study in 2017 found of all emergency department workers, nurses were the most likely to have been physically assaulted in the last six months and were less likely to feel safe. Nearly 60% reported verbal abuse and 12% were physically assaulted in the week prior to the survey.
Though this data tells a story of hospitals as a risky workplace, it’s difficult to grasp the entire scope of the problem. There is no regulatory requirement for healthcare workers to report incidents of violence, and each organization has its own policies and procedures. Each hospital reports this data differently to outside entities, making it difficult for researchers to compile and analyze data.
There is also a culture within healthcare that workplace violence is an inevitable part of the job. Nurses often consider physical violence a symptom of their patient’s illness, so they don’t submit incident reports. Working together, these barriers give the perception that violent incidents are routine, and therefore do not need to be treated.
Violent incidents can feel subjective, presenting another barrier to reporting. Is verbal abuse workplace violence? How about sarcastic or threatening language? How does bullying look and feel? Is this incident serious enough to report? Working within a culture that often accepts violence as “a day in the life,” it’s no wonder research shows only 20 to 60% of nurses report incidents of violence.
Research in 2015 studied the 12-month prevalence of violence in six U.S. hospitals. In that time, more than 2,000 workers reported 1,180 physical assaults, 2,260 physical threats, and 5,576 incidents of verbal abuse. Only 19% of events were reported into official reporting systems.
Without enough support or resources to handle the realities of violence in the workplace, nurses have lower staff morale, higher turnover, and increased reports of burnout. In fact, though 81% of nurses are satisfied with their career choice, 66% are worried their job is affecting their health, and 44% often feel like quitting.
Read the results of our 2019 survey on clinician burnout in healthcare >>
Legislation and looking forward
There is recent movement to recognize and improve workplace violence against hospital staff.
In late 2019, the U.S. House of Representatives approved the
A 2019 report released by the American Nurses Association stated, “The rate of violence against health care workers has reached epidemic proportions,” and proposed a multifaceted strategy to combat workplace violence. The recommendations ask for a focus on:
- Stopping violence before it occurs though education and identifying risks
- Immediate and effective response to violence
- Intervention to reduce long-term negative effects of workplace violence
Spok and Spectralink are partners in providing solutions to quickly alert nearby staff members and/or the security team of safety events, ensuring the appropriate help can arrive and resolve the situation quickly. Learn more about our partnership. You may also be interested in Spectralink’s post, In Healthcare, Taking Care of Business Starts by Taking Care of Caregivers.
To learn more about how to build a culture of safety and prevent workplace violence, OSHA has a wealth of resources for hospitals.
See a list of resources to explore to help create a safer work environment in part two in our series on workplace violence in healthcare.